Keratoconus is an eye condition in which the typically spherical cornea thins and bulges like a cone. Keratoconus usually affects both eyes, with one impacted more severely than the other. Your ophthalmologist Casper may do the following tests to detect keratoconus in addition to a comprehensive medical history and eye exam:
- Corneal topography: This is the most accurate approach to diagnosing and tracking the course of early keratoconus. A digital picture is obtained to map the cornea’s curvature.
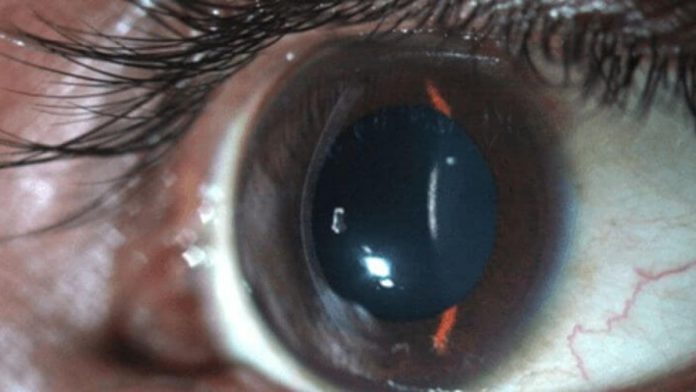
- Slit-lamp examination: This evaluation of the cornea can assist in discovering abnormalities in the cornea’s outer and middle layers.
- Pachymetry: This test determines the thinnest parts of the cornea.
- Keratometry: It is a diagnostic tool used to detect the degree and axis of astigmatism by measuring the curvature of the anterior portion of the cornea.
Symptoms of keratoconus
Keratoconus is distinguished by a thinning of the cornea, which alters its normal dome shape. It is usual to have no symptoms in the early stages of keratoconus. Asymmetry of your cornea can cause blurred vision and mild to severe distortion of your vision as the problem worsens. Early symptoms of keratoconus include:
- Rizzuti sign: A sharply curved reflection seen by shining a light on the side of the cornea closest to your temple.
- Fleischer ring: A brown ring of iron accumulation around your cornea that’s particularly visible with a cobalt blue filter.
- Vogt’s striae: Vertical lines observed on your cornea normally vanish when strong pressure is applied over your eye.
Causes of keratoconus
Keratoconus has been studied for decades, although it is still poorly understood. The exact cause of keratoconus is unknown; however, a predisposition to the condition is believed to exist at birth. The loss of collagen in the cornea is a common feature of keratoconus. This might be due to an imbalance in the synthesis and breakdown of corneal tissue by corneal cells.
Can keratoconus impair your vision?
Keratoconus, if left untreated, can result in irreversible vision loss. The corneal alterations make it difficult to focus the eye with or without eyeglasses or conventional soft contact lenses. Keratoconus is harmful if laser vision correction surgery, such as LASIK, is done on the eye since it can exacerbate the disease. Anyone with mild keratoconus should avoid laser vision correction surgery unless the physician recommends it.
Is surgery required if you have keratoconus?
Many keratoconus patients will never require a cornea transplant. Corneal crosslinking is a significant advancement in slowing or halting keratoconus, and therapy is vital to consider, particularly in young individuals with keratoconus, to reduce vision loss.
Surgery may be advised when glasses or contact lenses no longer fix your eyesight. Keratoconus patients often benefit from cornea transplantation surgery; however, it may take more than a year for eyesight to settle for you to benefit from new glasses or contact lenses. After a corneal transplant, some individuals still require a specialist contact lens to get their best vision.
Keratoconus is a disorder that impacts the cornea, the transparent dome-shaped portion of the eye. Because of this weakening, your cornea loses its characteristic dome shape, which can cause visual distortion. It often develops in adolescence and early adults and progresses for 10 to 20 years before stabilizing.
Diagnosis and treatment of keratoconus in its early stages provide you the best chance of reducing irreversible visual impairments. Call Cory Bergman, MD to schedule your consultation today to determine your ideal keratoconus therapies.